60/F WITH ACUTE GASTROENTERITIS
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Here is a case I have seen
Unit 6:
Case admitted on 27/2/2021.
Interns
K. Nikhil reddy
M. Swarna
K. Divya
B.Manivarma
Juveria
Dr. Vinay(pgy1)
Dr. A. Vaishnavi (pgy2)
Dr. Praneeth(pgy3)
Dr. Hareen (SR)
Dr.Praveen Naik( asst.prof.)
Dr.Rakesh Biswas (HOD)
A 60 year old female, shepherd by occupation came with Chief complaints of vomiting, loose stools since yesterday.
Patient was apparently asymptomatic since yesterday,later she complaints of vomitings since yesterday, 4-5 episodes/day , contains food particles,non bilious,non blood stained,subsided now.
Loose stools since yesterday, 4-5 episodes , rice watery stools,small amount multiple times , non blood stained,non foul smelling. Associated with pain in epigastric region , colicky type , no aggravating and relieving factors.
No H/o fever, melena.
No H/o recent travel, No H/o outside food consumption.
No H/o abdominal distension, burning micturition.
Past history:
H/o pain abdomen for 1-2 days, 20 days back, no vomitings, no loose stools.
Not a k/c/o DM, HTN , TB, asthma, epilepsy, CVA, CAD,thyroid.
No addictions.
Local examination:
Dry tongue+.
Pallor+.
No icterus, cyanosis, clubbing, lymphadenopathy,pedal edema.
Temp: afebrile
PR :84 bpm
BP:100/70 mmhg
RR: 18cpm
Spo2:97% at room air.
Systemic examination:
P/A: soft, tenderness noted in epigastric region.
Bowel sounds+.
CVS: S1,S2 heard, no murmurs
RS: BAE+, NVBS heard.
CNS: NAD.
Investigations:
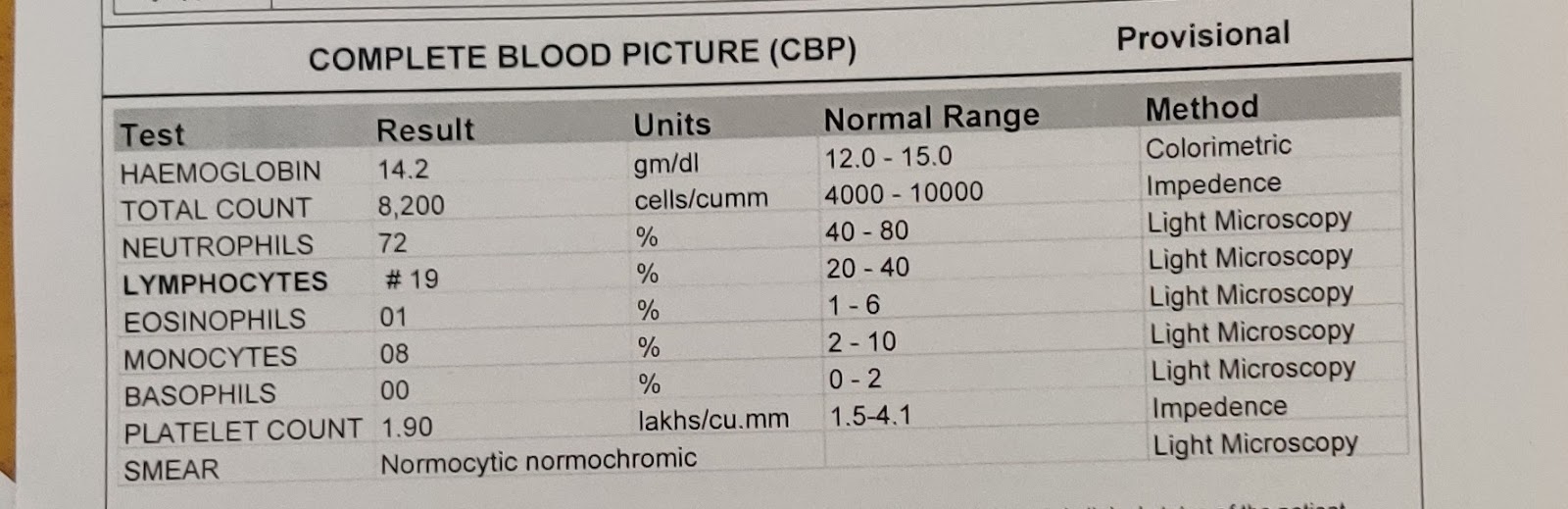
Hemogram
CUE
LFT
RFT
USG ABDOMEN
PROVISIONAL DIAGNOSIS:
ACUTE GASTROENTERITIS
Treatment given:
1.IV FLUIDS 2NS, 1 DNS, 1 RL @ 100ml/hr.
2.INJ. PANTOP 40 mg /po/OD..
3. INJ.ZOFER 4 mg/IV/TID
4. TAB. SPOROLAC -DS PO/TID.
5. ORS SACHETS 1 PACKET IN 1 LITRE , 200ML AFTER EACH STOOL.
6 INJ. BUSCOPAN 1 IV /SOS
7. TAB. CIFLOX 500MG PO/BD
8. INJ. METROGYL 500 MG /IV/TID
9. BP, PR CHARTING 2ND Hrly.
On 28/2/2021.
S: Stool frequency decreased, pain abdomen decreased,. No fresh complaints
O: patient is conscious, coherent, cooperative.
Temp:Afebrile
BP:120/80 mmhg
PR: 84bpm
RR:18cpm
P/A: soft, non tender
CVS: S1,S2 heard, no murmurs.
RS:BAE+, NVBS HEARD.
A: ACUTE GASTROENTERITIS
P: 1.IV FLUIDS 2NS, 1 DNS, 1 RL @ 100ml/hr.
2.INJ. PANTOP 40 mg /po/OD..
3. INJ.ZOFER 4 mg/IV/TID
4. TAB. SPOROLAC -DS PO/TID.
5. ORS SACHETS 1 PACKET IN 1 LITRE , 200ML AFTER EACH STOOL.
6 INJ. BUSCOPAN 1 IV /SOS
7. TAB. CIFLOX 500MG PO/BD
8. INJ. METROGYL 500 MG /IV/TID
9. BP, PR CHARTING 2ND Hrly.
On 1/3/2021
S: Stool frequency decreased, pain abdomen decreased,. No fresh complaints
O: patient is conscious, coherent, cooperative.
Temp:Afebrile
BP:110/80 mmhg
PR: 86bpm
RR:18cpm
P/A: soft, non tender
CVS: S1,S2 heard, no murmurs.
RS:BAE+, NVBS HEARD.
A: ACUTE GASTROENTERITIS
P: 1.INJ. PANTOP 40 mg /po/OD..
2. INJ.ZOFER 4 mg/IV/TID
4. TAB. SPOROLAC -DS PO/TID.
5. ORS SACHETS 1 PACKET IN 1 LITRE , 200ML AFTER EACH STOOL.
6 TAB. CIFLOX 500MG PO/BD
7. INJ. METROGYL 500 MG /IV/TID
8. BP, PR CHARTING 2ND Hrly.
Patient discharged on 2/3/ 2021 on request.









Comments
Post a Comment